Heart and Circulation
Reverend Dr. David C.M. Taylor
dcmt@liverpool.ac.uk
The aim of this page is to act
like a "virtual handout". It is not a complete overview
of the subject, but it should help you to direct your reading
and discussions. Any of the standard texts in your reading list
will help you to make sense of this subject. You might also like
to check my ECG web page.
These pages are © David Taylor/The
University of Liverpool, 2003.
Pacemaker activity
Cardiac Action
Potentials
Intrinsic Control
Extrinsic Control
Interaction
Cardiac Output
Factors affecting
stroke volume
Preload
Starling’s
Law
Contractility-"Inotropic
effect"
Afterload
Heart Rate
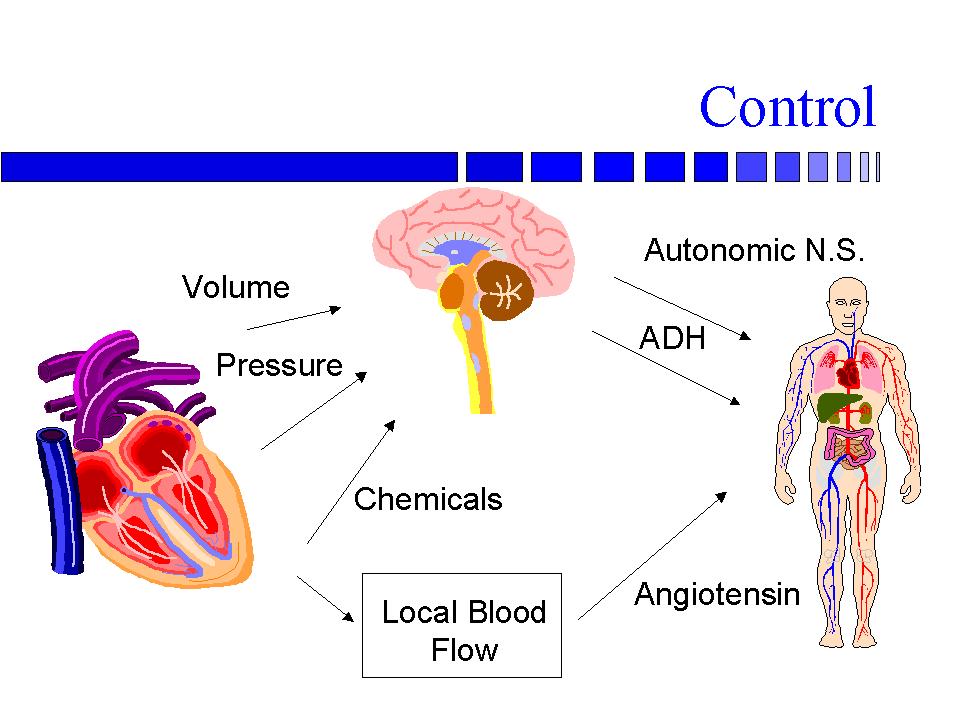
Control
Pressure
Volume
Chemicals
Local Blood Flow
(kidney)
Hormones
Overview
- The blood is pumped from the
left ventricle
- around the body to the right atrium
- and passes into the right ventricle
- From the right ventricle
- the blood is pumped around the lungs
- to the left atrium
- and then it passes to the left ventricle
Pacemaker activity
- The rhythm of the pump is provided
by the pacemaker activity of some specialized muscle cells in
the wall of the right atrium - the sinoatrial node
Cardiac Action Potentials
- The most obvious thing is that
they last longer than those in ordinary muscle
- This is partly due to the plateau
(arrow) due to an inward Ca2+ current
No Tetanus
- the action potentials last so
long there is no possibility of tetanus
Control
- is both intrinsic and extrinsic
Intrinsic
- The heart contracts more strongly
when it is full of blood
Starling’s Law of the
Heart
- The force of contraction is
proportional to the initial fibre length
Extrinsic Control
- The sympathetic system
- increase in the rate and force
of contraction largely through increasing the permeability of
cardiac muscle cells to Ca2+
- The parasympathetic system
- decrease in the rate of contraction
by slowing the pre-potential of the pacemaker cells.
- changes in heart rate are called
chronotropic changes
- changes in the force of contraction
are called inotropic changes
Interaction
- extrinsic and intrinsic systems
interact
Cardiac Output
- Heart rate x stroke volume
Factors affecting stroke volume
Preload
- increased end-diastolic volume
stretches the heart
- cardiac muscles stretch and
contract more forcefully
- Frank-Starling Law of the heart
Starling’s Law

Contractility-"Inotropic
effect"
positive inotropic agents
- increase available intracellular
Ca2+
- increase number of actinomyosin
binding sites
- increase force of contraction
- positive inotropic agents are
- sympathetic stimulation
- catecholamines
- glucagon
- thyroid hormones
- increased extracellular Ca2+
Afterload
- decreased arterial blood pressure
during diastole
- decreased afterload
- semilunar valves open sooner
when blood pressure in pulmonary artery & aorta is lower
- afterload is due to
- blood pressure
- viscosity of blood
- elasticity of arteries
Heart Rate
- Nervous system
- increased sympathetic
- decreased parasympathetic
- Chemicals
- catecholamines
- thyroid hormones
- moderate Ca2+ increase
- Other factors
- age
- gender
- "fitness"
- body temperature
Control
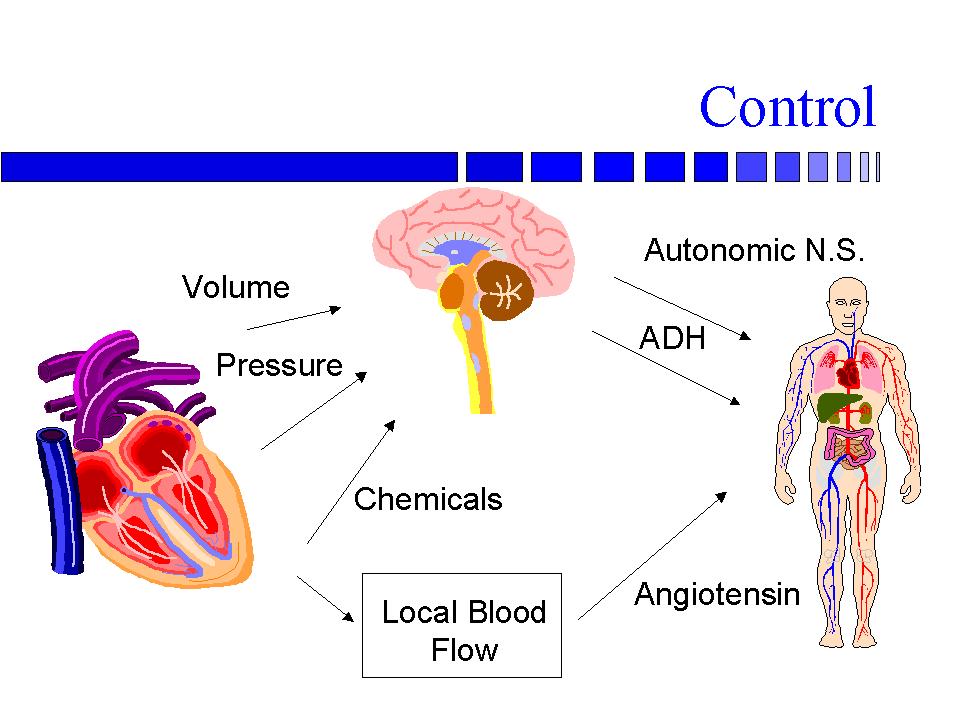
Pressure
- Sensed by baroreceptors
- in carotid arteries and aortic
arch
- an increase in pressure causes
a decrease in sympathetic activity
- a decrease in pressure causes
an increase in sympathetic activity
Volume
- Sensed by atrial volume receptors
an increase in volume
- causes a decrease in ADH secretion
- and an increase in ANF secretion
Chemicals
A decrease in O2,
or more usually an increase in CO2 or H2
causes an increase in chemoreceptor
activity which
- increases sympathetic activity
Local Blood Flow (kidney)
Hormones
- Angiotensin II is a vasoconstrictor
- Aldosterone increases vascular
sensitivity to Angiotensin II
- ADH (anti-diuretic hormone)
increases water reabsorption
- ANF decreases sodium reabsorption
Back to top | Back
to index